Welcome to the Breast and Cervical Cancer Treatment Program
The Department of Health Care Services implemented the Breast and Cervical Cancer Treatment Program (BCCTP) on January 1, 2002. The law that created the program was Assembly Bill 430 Chapter 171, Statutes of 2001.
The program provides cancer treatment benefits to eligible low-income California residents diagnosed with breast and/or cervical cancer.
BCCTP Applicant or Beneficiary Section
Can I get BCCTP benefits?
Eligibility
You may qualify for BCCTP benefits if:
- You live in California and
- Your gross (before taxes) family income, based on family size, is 200% of the Federal Poverty Level (FPL) or below at the time of application.
FPL chart
- You are found to be in need of breast and/or cervical cancer treatment.
You may also qualify to have an
Every Woman Counts (EWC) or
Family Planning, Access, Care and Treatment (Family PACT) provider screen and diagnose you, and help you apply for BCCTP.
Note: If you have other health insurance and your provider confirms you need cancer care, you can still apply for BCCTP coverage.
You may qualify for Federal BCCTP (full-scope Medi-Cal benefits) if you are:
- Uninsured,
- Under age 65,
- Under 200% FPL based on family size,
- A U.S. citizen or national or have satisfactory immigration status, and
- Found to need breast and/or cervical cancer treatment.
If you do not qualify for Federal BCCTP, you may qualify for State BCCTP (limited-scope BCCTP benefits) if you are:
- Uninsured or have other health insurance such as Medicare or private insurance,
- Any age,
- Under 200% FPL based on family size,
- Not a U.S. citizen or national or do not have satisfactory immigration status, and
- Found to need breast and/or cervical cancer treatment.
As of May 1, 2022, if you meet the points above and are age 50 to 65, you may qualify for full-scope benefits. Even if you do not have satisfactory immigration status.
Presumptive Eligibility
The Presumptive Eligibility (PE) program allows people applying for BCCTP benefits to get temporary care and treatment right away.
- These temporary benefits start the day you apply. They end the last day of the next month if you do not apply for Medi-Cal at your County Social Services office by that day.
-
PE will extend if you apply for Medi-Cal at your County Social Services office by the last day of the month after the month you applied for PE.
You will not get PE benefits if one of these is true:
- Age 65 or older,
- Have Medicare or private health insurance,
- Had hospital emergency or pregnancy PE benefits within the last 12 months, or
- Are identified in the Medi-Cal database as having unsatisfactory immigration status.
You must apply for Medi-Cal at your County Social Services office to keep your temporary PE benefits active. Once the county decides if you qualify for Medi-Cal, you will get a letter. If you do not qualify for Medi-Cal through the county, they will send your information to BCCTP.
If you apply for Medi-Cal
after PE has ended, you should re-apply for BCCTP. Ask the medical provider, who helped you apply, to submit another application for you. Or, you can also ask the county eligibility worker to send your information to BCCTP.
What are the BCCTP benefits?
Federal BCCTP (full scope Medi-Cal) benefits cover breast and/or cervical cancer treatment and related services. They also include other non-cancer health care services.
State BCCTP (limited scope Medi-Cal) benefits
cover breast and/or cervical cancer treatment and related services.
If you are in BCCTP, you can learn what health care services are covered by calling
Member Benefits/Provider Support at 800-541-5555.
If you have other health insurance
such as Medicare or private insurance and your premiums, co-pays and deductibles are expected to be more than $750 per year, you may still qualify for State BCCTP benefits.
You may qualify to get your health insurance premium costs paid back to you. The Department of Health Care Services' Health Insurance Premium Payment (HIPP) program pays you back for your health insurance premium costs four times a year. BCCTP will tell you if you qualify for the HIPP program.
How long do BCCTP benefits last?
BCCTP benefits will stay active as long as you need cancer treatment and meet all other BCCTP eligibility rules. BCCTP will send you a redetermination packet when it is due. You must return the completed packet to find out if you still qualify.
How can I apply for BCCTP?
You can apply for BCCTP Medi-Cal in one of three ways:
- A Cancer Detection Program (CDP): Every Woman Counts (EWC) provider can submit the application for you. To find an EWC provider visit the Every Woman Counts page.
- A Family Planning, Access, Care and Treatment (Family PACT) provider can submit the application for you. To find a Family PACT provider visit the Family PACT page.
- A County Eligibility Worker (CEW). If you have Medi-Cal through your County Social Services office, tell the CEW you have breast or cervical cancer and want your information sent to BCCTP. If you do not have Medi-Cal with the county, you must apply for Medi-Cal at your County Social Services office, tell the CEW you want your information sent to BCCTP.
- If California is in a Public Health Emergency, please visit the
Information Page for Beneficiaries & Members.
You can apply for Medi-Cal at your County Social Services office by mail, in person, or online.
Apply for Medi-Cal.
What happens after I apply for BCCTP?
If you applied for BCCTP through an EWC or Family PACT provider's office, you also have to apply for Medi-Cal at your County Social Services office. If you applied for Medi-Cal within the last 30 days before you applied for BCCTP or you have Medi-Cal through your county now, you do not need to re-apply for Medi-Cal. If you were approved for PE, you can use that temporary coverage while the county and BCCTP decide if you qualify.
After you apply for BCCTP, an Eligibility Specialist may contact you and ask for more information. They might ask for proof of income, your family size, and information about other health insurance coverage. BCCTP will mail you a letter with the BCCTP decision. The letter will explain your eligibility or the reason you did not qualify for BCCTP. You may also get a Benefits Identification Card (BIC) in the mail. It looks like this:
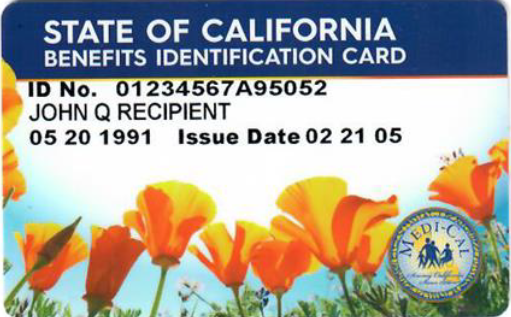
You should show your BIC at all medical appointments. Also, show it when you pick up prescriptions at the pharmacy. Your providers use it to view your Medi-Cal benefits and see if your services are covered.
What is Retroactive Medi-Cal?
If you got medical treatment or services before you applied for BCCTP, Medi-Cal may cover the cost of your care for up to
90 days before your application date. This is called “retroactive benefits." You can ask BCCTP for an application for retroactive benefits. You must apply within 12 months from when you got the service.
To qualify for retroactive benefits, you need to qualify for BCCTP benefits. You must have also met all of these eligibility rules during the time period for which you are requesting retroactive benefits:
- Were under age 65;
- Had:
- Been screened and found in need of treatment by Every Woman Counts (EWC) or Family PACT provider, or
- Had any breast and/or cervical cancer-related clinical services, including treatment and diagnosis, done by an EWC or Family PACT provider;
-
Did not have health insurance covering breast and/or cervical cancer treatment;
-
Lived in California;
and
-
Got services from a Medi-Cal provider at any time during the three-month period right before the month you applied for the BCCTP.
If you are not a U.S. citizen or U.S. national, or do not have satisfactory immigration status during the retroactive eligibility months, your retroactive benefits are limited to Medi-Cal emergency and pregnancy-related services.
My BCCTP Benefits
I got a BCCTP Annual Redetermination packet. What do I do?
When you are approved for BCCTP benefits, you must update your information each year to keep your benefits. The BCCTP Eligibility Specialist will send you the packet each year. Complete and return the papers in it to BCCTP. You must return the packet by the due date in the letter so BCCTP can decide if you can keep your benefits for another year.
If you do not have Medi-Cal benefits through the county,
you must complete a Medi-Cal application with your local County Social Services office. You can apply online, by phone, or in person. To find your local Medi-Cal office, please call 1-800-541-5555 or visit the
County Offices website, or
apply for Medi-Cal online. If you already have county Medi-Cal, you do not need to reapply.
Annual Redetermination Requirement (Federal and State BCCTP)
These papers are in the Annual Redetermination packet:
-
The Continuing Eligibility Redetermination form: This form asks for your current contact information, income and family size. It also asks if you have other healthcare insurance, such as Medicare. And it asks if your citizenship or immigration status changed.
-
A Physician Statement and Certification form: The doctor treating your cancer must complete and sign this form. It certifies that you still need treatment for breast and/or cervical cancer.
-
Patient Information and Authorization for Release of Protected Health Information: This form lets you allow your doctor to release protected health information to the BCCTP.
-
Rights and Responsibilities: This form is for information and your records. It explains your rights and responsibilities as a Medi-Cal beneficiary.
Make sure you return all completed and signed paperwork by the due date. If you do not, your benefits may end.
Return by:
Fax: (916) 440-5693
Mail: Department of Health Care Services
Medi-Cal Eligibility Division
Breast and Cervical Cancer Treatment Program
P.O. Box 997417, MS 4611
Sacramento, CA 95899-7417
What changes eligibility?
Eligibility changes for the reasons below. With each change,
BCCTP will send a copy of your case to your County Social Services office. They will review your Medi-Cal eligibility. They will tell you if you qualify for another Medi-Cal program. If the County finds that you do not qualify for any Medi-Cal program, they will tell BCCTP.
-
You turn age 65: BCCTP will review your case for State BCCTP (limited-scope Medi-Cal) benefits. The State BCCTP benefits only cover breast and/or cervical cancer treatment and related services.
-
You get other health insurance, including Medicare: BCCTP will review your case for State BCCTP (limited-scope Medi-Cal) benefits. The State BCCTP benefits cover breast and/or cervical cancer treatment and related services. They also cover co-pays and deductibles. You may qualify to have your health insurance premium costs paid back to you through the HIPP program.
-
Your doctor finds that you no longer need cancer treatment: BCCTP will send a copy of your case to your County Social Services office. They will review your Medi-Cal eligibility and will tell you if you qualify for another Medi-Cal program. If the county finds that you do not qualify for any Medi-Cal program, they will tell BCCTP and your BCCTP benefits will end. You will get a “discontinuance" letter.
Note: Your BCCTP benefits will
not change or end while the CEW finds out if you qualify for other Medi-Cal programs.
What happens if my immigration status changes?
If your immigration status changes, you will need to tell the BCCTP. BCCTP will tell you if you qualify for Federal BCCTP (full-scope Medi-Cal) benefits.
I have BCCTP benefits and need help with:
Billing:
I received a medical bill that BCCTP didn't cover.Call
Member Benefits/Billing
at (800) 541-5555.
If you recently applied for BCCTP, once you get a BCCTP approval letter you can call the provider on the bill and discuss Medi-Cal payment.
Dental
benefit questions:
Call Medi-Cal Dental Program at (800) 322-6384
Estate Recovery Services: I got information about Estate Recovery and have questions.
Contact the
Estate Recovery office at (916) 650-0590 or email
ER@dhcs.ca.gov
Health Insurance Premium Payment Program: It has been more than 90 days and my insurance premium payment has not been paid back to me.
Contact the
Third Party Liability & Recovery Division at the address below, by
FAX (916) 440-5676 or email
HIPP@dhcs.ca.gov.
Department of Health Care Services
Third Party Liability and Recovery DivisionHealth Insurance Premium Payment ProgramP.O. Box 997425, MS 4719
Sacramento, CA 94899-7422
Medi-Cal Managed Care Health Plan: I do not want to be in a health plan. Or, I want to change health plans.
Call the
Medi-Cal Managed Care Ombudsman Office
at
(888) 452-8609.
Medi-Cal RX: I have questions about prescriptions under Medi-Cal RX. Call 800-977-2273 or
email
Can I get treatment outside of the county I live in?
As of January 1, 2022, many persons receiving BCCTP benefits will have to get treatment in the county they live in.
To learn more about the Managed Care Plan(s) in your county, please see the Health Plan Directory (ca.gov)
Out-of-pocket payment: I paid for services that BCCTP should have covered.
Call the
Out-Of-Pocket Expense Reimbursement Unit (Conlan)
at
(916) 403-2007.
Prescriptions: BCCTP did not cover my prescription. Or, I have questions about my prescriptions.Call
Member Benefits at (800) 541-5555.
How to contact BCCTP
Phone: (800) 824-0088Email:
BCCTP@dhcs.ca.govFax: (916) 440-5693Mail: Department of Health Care Services Medi-Cal Eligibility Division Breast and Cervical Cancer Treatment Program P.O. Box 997417, MS 4611
Sacramento, CA 95899-7417
Resources for health insurance and cancerIf you do not qualify for BCCTP, you can apply for insurance affordability programs through the Covered California website here:
(www.CoveredCA.com).
Covered CA's toll-free number: (800) 300-1506 (TTY: (888) 889-4500)
Resources not linked to Medi-Cal:
Social Security Administration (800) 772-1213
Medicare (800) 633-4227
The American Cancer Society (800) 227-2345
Susan G. Komen Breast Care Helpline: (877) 465-6636
